Response to ABC's 4Corners Program
A Response to the Australian Broadcasting Corporation's '4Corners' Program on Metal-on-Metal Hips.
On the 16th of May 2011, the ‘4Corners’ program on the Australian ABC Channel aired a documentary relating to patients who underwent hip resurfacings and highlighted the problems being faced by patients who were implanted with an ASR resurfacing.
We agree fully with Professor Ross Crawford of Australia and with Quentin McDermott the presenter that ‘historically, hip replacements are among the Western world's most popular and successful operations.’
We also agree that there are many fundamental flaws in the ASR design and its materials, as there are with some other designs of resurfacings. We spotted these design problems at the outset and have been highlighting them to the world for the past six years, long before the resultant clinical problems actually came to light. We extensively debated the issue in great detail in what has come to be called ‘The Northern Lights Debate’ in Finland. A multimedia version of the debate has been on our website ever since and has been viewed by the thousands who have visited our website. We also presented our concerns in early 2006 at the American Academy of Orthopaedic Surgeons in Chicago. With regards to materials issues, we have been fighting for quality control since 1996 when heat treatments were first introduced in artificial hip devices, for the first time in the history of hip replacements.
The 4Corners program itself however does not represent a balanced ‘take’ on the subject. This was not unexpected in a media presentation of this nature but it is important to point out why the program is more sensational than educational.
While presenting true stories of patients who had problems with ONE device produced by ONE company, the obtuse references to metal-on-metal in general from time to time misinforms the public that all metal-on-metal resurfacings are terrible.
Specifically they do not refer to the results of the BHR which has been in use for at least twice as long as the ASR, and with far greater numbers than the ASR, to check if the ASR results can be generalized to all MoM hips.
Most importantly the program does not explore what the alternative options are (if a resurfacing is not performed on young active patients with arthritic hips), and whether there are any downsides to treatment options like total hip replacements using ceramic or polyethylene bearings.
  For the sake of clarity, we feel it is necessary to present some facts from the past and from current scientific reports and from the large National Joint Registers, which are powerful unbiased reports of device performance. For the sake of clarity, we feel it is necessary to present some facts from the past and from current scientific reports and from the large National Joint Registers, which are powerful unbiased reports of device performance.
There are over 20 different resurfacing brands in the market and an even greater number of metal-on-metal hip replacements. It must be stated that all resurfacings are NOT the same. The terrible results of a resurfacing like the ASR cannot be applied to all the others. Nor can the good results of a resurfacing like the BHR be applied to others.
I declare that I do not receive royalties for the BHR nor do I own shares and stocks in the company that produces them. As the inventor of the BHR I declare at the outset that my interest relates to the Birmingham Hip Resurfacing (BHR) but we shall present as unbiased a picture as possible.
How long have the current generation of metal-on-metal (MoM) resurfacings been in use? Has there been due testing before their introduction?
There is a perception that all metal-on-metal (MoM) resurfacing devices have been introduced into clinical usage without much thought or testing. That is true for many recently introduced resurfacings, but not true for the BHR.
It is 3 months since we at the McMinn Centre celebrated the 20th anniversary of the first modern MoM resurfacing. Since then we have reviewed several patients for their 20-year follow-up and some of those early devices are still functioning well.
I started working on hip resurfacings in the late 1980’s in Birmingham. The scientific basis for this was provided by the observations made on MoM total hip replacements which had been in place for 20 to 30 years, and by the knowledge gained from the failure of previous attempts at resurfacings.
I obtained some of the successful metal components and had them carefully analyzed. Their beneficial design features and materials were incorporated into my earliest concept models. After further tests we implanted the first modern metal-on-metal (MoM) resurfacing in February 1991, with the patients fully understanding that although this was uncharted territory it had been carefully thought through and well-considered.
 During the next six years we conducted several studies to assess the viability of the femoral head after resurfacing, to determine the best method of fixation of the implants and the effects of metal wear. Further potential problems with the design and material processing of these devices were meticulously identified and addressed in subsequent models, until the introduction of the Birmingham Hip Resurfacing (BHR) in 1997 as a product based on the many lessons learnt during those years. During the next six years we conducted several studies to assess the viability of the femoral head after resurfacing, to determine the best method of fixation of the implants and the effects of metal wear. Further potential problems with the design and material processing of these devices were meticulously identified and addressed in subsequent models, until the introduction of the Birmingham Hip Resurfacing (BHR) in 1997 as a product based on the many lessons learnt during those years.
From 1991-1996 the device had largely been used by a few of us hip surgeons in Birmingham and not released for general usage. Dr Graham Mercer from the Australian Orthopaedic Association and Dr Rohan Hammett from the Australian regulatory body TGA suggested that implants should be tested for 2 years before being released. We had worked on the device in Birmingham for over 6 years and perfected it in a steady step-wise manner before releasing it for general use.

After the BHR was introduced, a training program was instituted for surgeons and further studies were started. These relate to hip function, metal ions, implant migration, stress shielding, the effects of resurfacing and replacement on the coagulation cascade and the best form of thromboprophylaxis, to name a few.
As the years passed, patients and surgical colleagues saw the outstanding results in young and active patients and overcame the initial scepticism relating to the potential problems with MoM. Till then patients undergoing hip replacements were almost universally advised to give up high activity in order to allow the hips to last. After having a BHR, patients were advised to carry on activity as normal. The operation not only restored hips to a pain-free status but allowed some of the patients to return to phenomenally high activity levels and regain their lost dreams and goals in life, including in some cases world championship-level sport, even in certain high impact sports.
What about other MoM resurfacings?
It has been said that "imitation is the sincerest form of flattery", and the success of the BHR eventually led to the independent development of several metal-on-metal resurfacings by large commercial companies. This is when problems arose.
One of these introductions was the ASR, a device designed by a group of engineers and surgeons. With all good intentions they introduced certain conceptual improvements which are great if viewed in isolation. However, in surgical interventions every change comes with the price of potential adverse effects. Because of our earlier experience with resurfacing device introduction we were able to immediately spot these problems. Very early we started to speak up about these problems warning colleagues in conferences and warning the public through our website, even under threat of legal action by vested interests. It is sad that those unheeded warnings are now coming true.
Other resurfacings had other problems. Another orthopaedic company called Zimmer introduced the Durom Resurfacing. This also ran into problems because amongst other things the implanted cups did not integrate into bone and started becoming loose from the bone. The alarm was raised by a leading surgeon in the USA. The cup also was designed with a sharp edge which led to patients complaining of groin pain when their muscles started rubbing against the edge. The company eventually withdrew the product from the US market.
What are the current results of the BHR in the National Joint Registers?
The Australian and the UK National Joint Registers together comprise the largest unbiased documentation of artificial joint devices in the world. The BHR has the longest follow-up and the largest number of resurfacing cases included in both these Registers.
The Australian Register has over 9000 BHRs with a 9-year success (implant survivorship) rate of 93.8% overall including all ages and both genders. This is despite the fact that the BHR is used commonly in younger more active patients. In men the 9-year BHR survivorship is 95.2% in all ages which compares favourably with total hip replacements. And of course, the best results are seen in young men, the very age group for which the device was originally developed. It must be understood that national registers include the results of all surgeons, highly experienced, not so experienced and trainees. In my hands the BHR survivorship at 13 years and 10 months is 97% overall and 98% in men. Other devices including the Durom and the ASR have 5-year results on the Australian Register and they already show 2 to 3 times higher failure rates than the BHR.
The UK Register which was instituted more recently provides 5-year survivorship data. Over 8000 BHRs are included and the 5-year survivorship is 95.7% overall. In comparison the Cormet 2000 and the ASR show 90% and 88% 5-year survivorship.
The Resurfacing Register maintained by the Oswestry Outcomes Centre in the UK is the longest-running Resurfacing Register and tracks the history of 5000 BHRs from over 141 surgeons around the world and they show a survivorship of 95% at 10 years for the BHR. This includes surgeons of all levels of experience from around the world.
What are the results of ASR and other MoM resurfacings?
The ASR and the Durom were introduced as low clearance resurfacings. Both of these devices showed higher failure rates than the BHR in the Australian Register. The UK Register also shows the ASR and the Cormet resurfacings are performing worse than the BHR.
The ASRXL was introduced as a low clearance MoM THR which has also has been showing high failure rates in the Australian and UK Registers.
One Centre in the UK reports a failure rate approaching 25% with ASR resurfacings and 50% with ASR XL total hip replacements at 7 years. Many of these are related to excess wear. Some have termed these "pseudotumours" even though they have nothing to do with tumours.
Other series from the same region had 14% debris-related failures with ASRs at 7 years compared to less than 2% failure rate with BHRs at 11 years.
What are metal debris-related failure rates in BHRs?
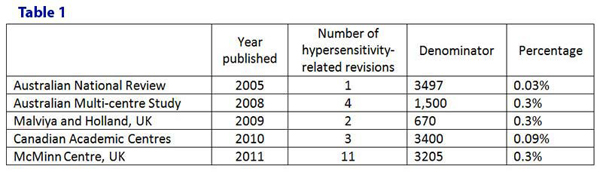
In terms of adverse reaction to metal wear products, in our series of over 3200 BHRs a very small percentage (0.3%) only have been revised. On average they had pain-free hip function for nearly 9 years after their BHR implantation. They have been revised to a traditional hip replacement and are back to their normal activity levels. There have been no muscle group necrosis, pathological fractures or dislocations. None of them had cobalt toxicity or strokes, cardiac problems, blindness, deafness or systemic organ failures. None of them has had to undergo a re-revision. This low incidence of "pseudotumours" is also reflected in several other large series in which the majority were BHRs (Table 1).
There was a report from Oxford where they experienced failures with several different types of resurfacings. Analysis of their explanted components showed that all of them had been malpositioned, thereby leading to edge wear and failure.
It must be noted however that modern artificial hip bearings whether metals or ceramics or modern polyethylenes, are all very sensitive to component malposition. They must be implanted well in order to enjoy long-term success. Malpositioning of components causes implant failure even if the best device is used.
Is this "the tip of an iceberg"? Are we going to see increasing numbers of patients with strokes and systemic organ failures with the passage of years?
What happens to the patients fitted with ASRs or recent resurfacings is not fully known because of the absence of historic provenance for these devices.
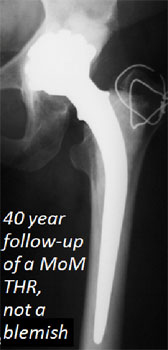
The BHR is based on the pedigreed design characteristics and materials of historic metal-on-metal hip replacements which had been in clinical use for several decades.
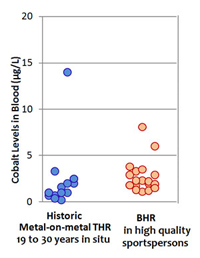
Very early after the introduction of the BHR we compared the cobalt levels of highly active patients who had had BHRs with the cobalt levels in patients who had historic cobalt-based metal-on-metal hip replacements performed 19 to 30 years before and found that the levels in these two groups were in the same range. Therefore we can expect with good reason that the BHRs will follow the progress of these historic devices.
4Corners presents one of Prof. Ross Crawford's "very, very active elderly lady" patients who developed a stroke four years after a DePuy ASR resurfacing as "first-hand evidence" that over the next few years we are going to face dangerous cobalt toxicity in patients with metal on metal hips.
Anyone looking for hard evidence in the world literature will find the published life work of Prof Visuri and colleagues in Finland. They studied more than 2000 patients with hip replacements over 30 years and compared their causes of death with the general population. The patients included 579 who had metal-on-metal (MoM) THAs and 1585 who had metal-on-poly (MPE) THAs, providing exposure risk of over ten thousand person-years with the MoM hips and over twenty six thousand person-years with MPE hips. Patient records from the general population were used as controls.
They found that there was no significant increase in cancer rates or in organ system failure rates with the exception that those with traditional hip replacements had a higher likelihood of dying from Alzheimers disease (Table 2). This was after 30 years and if there was a hidden iceberg under the surface at 5 years (as the 4Corners program suggests) we would expect it to surface in 30 years.
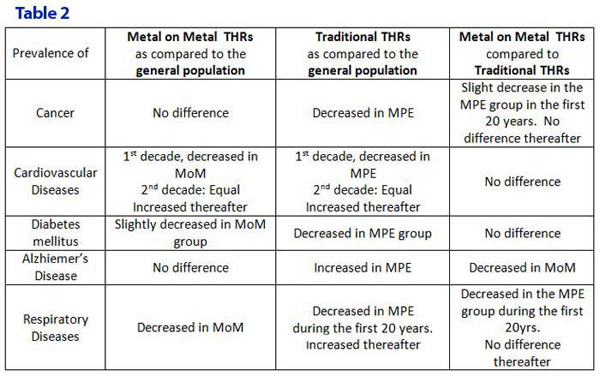
The effect of hip resurfacings and replacements on the incidence on systemic disease has also been studied in the large UK National Joint Register. It showed that both metal-on-metal (MoM) resurfacings and non-metal-on-metal (non-MoM) hip replacements led to higher incidence of renal cancers and hearing loss when compared to the general population, but there was no difference between the incidence when MoM resurfacings were compared to non-MoM hip replacements.
What then are the options for a young patient with hip arthritis? Are non-MOM replacements safer than MoM resurfacings?
As we have seen above there is no significant difference between MoM or non-MoM bearings in terms of cancer or systemic disease. The reason for our introduction of MoM resurfacings in young patients was because the failure rates of traditional hip replacements in the young were very high. The Swedish Register showed that in men with osteoarthritis under the age of 55 years, traditional hip replacements failed at the alarmingly high rate of 19% at 10 years and 67% at 16 years. This was worse than the revision rates of all resurfacings combined and much worse than the revision rates of the BHR in the UK and Australian Registers. These traditional hip failures were associated with much bone loss and progressively difficult revision operations. Our failure rate with the BHR in the same age group and diagnosis was 2% at 13 years.
There are no easy solutions for the young patient. With traditional hip replacements, the problems of multiple revisions and of multiple dislocations in active young patients can be very restrictive for a patient wanting to resume an active lifestyle.
Furthermore every hip device whether using a polyethylene bearing or a ceramic bearing has metal either in the stem and/or in the cup. It is just coming to light that with nonMoM hips as we try to extend bearing life through improved materials and as we increase the bearing diameter in order to reduce dislocations, metal can leech from the (taper) joint connecting the stem and the head or the cup and the insert and cause the same problems as seen with bad resurfacings.
What has shocked many in the orthopaedic community is a hitherto unidentified factor which the UK Register 2010 brought out. It finds that the mortality rate over the 5 years following hip resurfacing is phenomenally lower (1.8%) compared to that following hip replacements (9.9%). This benefit persists even after multivariable adjustment for age, gender and physical status. This suggests that traditional hip replacement adds some as yet unidentified detrimental effect to the patient as a whole, which the recipients of hip resurfacing appear to escape.
Total hip replacement in young patients comes with the price tag of a higher revision rate and a higher mortality rate. A well-designed, well-engineered, well-implanted resurfacing is a much better option than a hip replacement.
SUMMARY
Kerry O'Brien the presenter of the 4Corners program describes the ASR resurfacing as "the biggest disaster in the history of orthopaedics". Two decades ago, after studying the failed resurfacings designs of the 1980s, we came to the conclusion that "the bad results of resurfacings are the results of Bad Resurfacings." If the current debacle with resurfacings shows us one thing it is that we have not learnt from history.
There is now overwhelming evidence to demonstrate clearly that ASR was a badly designed resurfacing and was a disaster waiting to happen. The same evidence also demonstrates that the results of the BHR especially in young patients is very good, the very group who fare poorly with a traditional hip replacement. It would be unfortunate if the adverse results from a few ill-designed, poorly implanted devices are allowed to throw this excellent treatment option into disrepute.
The results show that BHR works well, especially in young and active patients. The BHR has been implanted in more than 140,000 patients worldwide and for twice the duration as the longest ASRs. These include professional athletes, firemen, members of the armed forces and even orthopaedic surgeons. It has restored their quality of life and returned them to their professions. One study found that over 90% of the resurfaced men participated in sporting activities and over 60% participated in impact sports without detriment to their artificial hip. As the inventor of the BHR, I am confident that this technology will stand the test of time as the published evidence has been proving.
It must be remembered however that component malposition is a cause of failure and should be avoided. Choose your device and your surgeon carefully. If you have any further questions or queries, please do not hesitate to contact us: enquiries@mcminncentre.co.uk
Derek McMinn MD FRCS
|